Introduction
In recent years, bariatric surgery has emerged as a potentially life-altering option for individuals grappling with obesity and related health concerns. Globally, an alarming 13% of the adult population is affected by obesity, a statistic that underscores the urgency of finding practical solutions for weight management[1]. Bariatric surgery, encompassing a variety of procedures such as gastric bypass and sleeve gastrectomy, offers a pathway to substantial weight loss and a bridge to a better quality of life by alleviating obesity-related comorbidities, including diabetes and hypertension[2].
But bariatric surgery is not a decision to be taken lightly. Apart from being a significant financial undertaking, it necessitates deep-seated lifestyle and emotional adaptations post-surgery. Research indicates that the road to recovery and adaptation demands a holistic approach to well-being, marrying physical changes with psychological readiness and a robust support system[3].
In this article, we probe the various dimensions of bariatric surgery, illuminating the potential benefits and delineating the risks involved. With expert insights and a rounded perspective, we will equip you with the information you need to decide to undergo bariatric surgery[4]. Is it the right choice for you? Could it be the key to a healthier body and a more fulfilling life?
As we chart this exploratory path, we invite you to join us in examining each facet of bariatric surgery with a critical eye, fostering an understanding grounded in research and expert opinions[5]. Step into this guided journey towards unlocking a better quality of life through bariatric surgery, steering your decision with comprehensive, reliable information.
Understanding Bariatric Surgery
Types of Bariatric Surgery
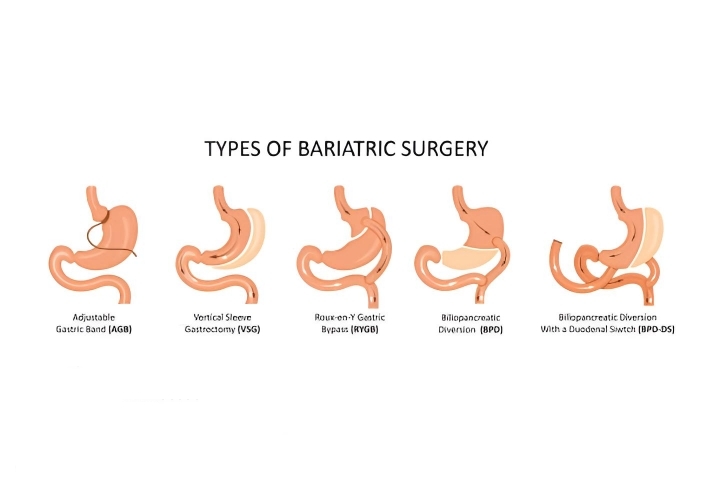
Bariatric surgery encompasses a range of procedures designed to aid in weight loss and improve the health outcomes of individuals with obesity. The primary types include:
- Gastric Bypass: This involves creating a small pouch from the stomach and connecting it directly to the small intestine, thereby bypassing a significant portion of the stomach and the first part of the small intestine[6].
- Sleeve Gastrectomy: Here, a substantial part of the stomach is removed, leaving a smaller, banana-shaped stomach that limits food intake[7].
- Adjustable Gastric Band: In this procedure, an adjustable band is placed around the upper part of the stomach, creating a small pouch that controls food intake[8].
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A more complex procedure where a part of the stomach is removed, and the remaining part is connected to the lower portion of the small intestine, bypassing a large part of the intestine[9].
How Bariatric Surgery Works
Each type of bariatric surgery functions slightly differently, but all aim to restrict food intake and/or reduce nutrient absorption, aiding in weight loss.
- Mechanism: The surgeries alter the digestive system to limit the amount of food one can eat, reduce the absorption of nutrients, or both. These changes facilitate reducing calorie intake, encouraging weight loss[6].
- Expected outcomes: While results can vary, many individuals experience a significant reduction in their body weight post-surgery. This is coupled with improvements in obesity-related comorbidities, such as diabetes and hypertension, enhancing the overall quality of life[5].
By understanding the underlying principles and outcomes associated with different types of bariatric surgery, individuals can better gauge whether this approach might suit their health needs and lifestyle goals.
The Benefits of Bariatric Surgery
Weight Loss
A primary benefit of bariatric surgery is substantial weight loss. Patients undergoing these surgeries can witness a notable reduction in body weight, facilitating a pathway to a healthier life. Studies have documented significant weight reduction, with patients losing, on average, 60% of their extra weight post-surgery. However, results can vary depending on individual circumstances and the type of procedure performed[10].
Success stories abound, with many individuals regaining mobility and enjoying a more active lifestyle after the surgery[11].
Improved Comorbidities
Bariatric surgery does more than aid in weight loss; it also plays a pivotal role in improving or even resolving obesity-related comorbidities, including:
- Diabetes: Bariatric surgery can significantly improve or remit type 2 diabetes, helping patients maintain blood sugar levels more effectively[12].
- Hypertension: Post-surgery, many individuals find a reduction in high blood pressure levels, fostering better heart health[13].
- Sleep Apnea: Weight loss through bariatric surgery can alleviate the symptoms of sleep apnea, promoting better sleep and reducing the risk of associated complications[14].
Enhanced Quality of Life
Besides physical benefits, bariatric surgery can substantially enhance one’s quality of life.
- Physical benefits: Individuals can lead a more active lifestyle, with improved mobility and less strain on joints[11].
- Psychological benefits: Many patients experience improved mental health, witnessing decreased symptoms of depression and anxiety post-surgery[15].
- Social benefits: With better physical and mental health comes improved social interaction, helping individuals forge more robust bonds and enjoy social gatherings without hindering mobility issues and self-esteem concerns[15].
Through bariatric surgery, individuals lose weight and gain a chance at a healthier, happier life with improved physical, psychological, and social well-being.
Risks and Considerations
Surgical and Post-operative Complications
Like all surgeries, bariatric procedures come with inherent risks. While these surgeries are generally considered safe, complications can occur:
- Infections: Surgical site infections are a possible risk, necessitating stringent post-operative care to prevent infections[16].
- Blood Clots: The surgery can lead to the formation of blood clots, which can be life-threatening if not addressed promptly[17].
- Nutritional Deficiencies: Given the alteration in the digestive system, patients might face nutritional deficiencies, requiring lifelong vitamin and mineral supplements[18].
Psychological Impacts
It’s also crucial to address the potential psychological ramifications post-surgery:
- Mental Health: While many find an improvement in mental health, others might face challenges, including issues with body image and relationships. Some patients even experience heightened anxiety and depression[3].
- Behavioral Changes: The dramatic lifestyle change can spur behavioural adjustments, including changes in eating habits, which might be stressful for some individuals[19].
Long-term Commitment
Embarking on the journey of bariatric surgery is a long-term commitment. Here are some aspects to ponder upon:
- Lifestyle Changes: Individuals must adhere to a strict diet and exercise regimen post-surgery to maintain the results[4].
- Follow-up Appointments: Regular follow-up appointments are crucial to monitor individual progress and address concerns[4].
Understanding the potential risks and making an informed decision based on a comprehensive consideration of the benefits and challenges is essential to ensuring the best possible outcome from a bariatric surgery.
Is Bariatric Surgery Right for You?
Medical Criteria
Bariatric surgery is a significant step and isn’t suitable for everyone. Medical professionals generally have a stringent set of criteria that individuals must meet before being considered for surgery. These criteria often include a Body Mass Index (BMI) of 40 or higher or a BMI of 35 or higher coupled with severe weight-related health issues, such as type 2 diabetes or high blood pressure[20]. In addition, individuals are usually required to demonstrate that they have tried and failed to lose weight through traditional methods such as diet and exercise[21].
Personal Considerations
Consultation with a Specialist
Before deciding, it is highly advised to consult with a specialist who can provide individualised advice based on one’s medical history and current health condition. This consultation generally involves a thorough evaluation to determine if bariatric surgery is the most suitable option for you[5].
Deciding to undergo bariatric surgery is a substantial commitment that involves carefully considering various factors. It’s a personal choice that should be made after carefully weighing the benefits and risks and consulting with a healthcare provider specialising in this field.
Beyond the medical criteria, potential candidates should consider personal factors, including:
- Mental Preparedness: Being mentally prepared for post-surgery changes is essential. Candidates should be ready to commit to a lifetime of healthy eating and regular physical activity[3].
- Support System: A reliable support system post-surgery can aid a smoother recovery and adjustment process. It helps to have family and friends who understand and support your journey[22].
Conclusion
In pursuing enhanced quality of life and better health outcomes, many are considering bariatric surgery a viable option. This life-altering decision, grounded in medical necessity and personal readiness, can potentially offer a fresh start to those grappling with severe obesity and associated health complications[20][5].
Nevertheless, it is pivotal to undergo this journey with full awareness and preparation, acknowledging both the opportunities for improvement and the challenges ahead. The rigorous medical criteria delineate the seriousness of this procedure, with an emphatic focus on the candidate’s overall health condition and readiness to adopt a new lifestyle post-surgery[21][3]. Furthermore, acknowledging the importance of a supportive network — be it family, friends, or healthcare providers — cannot be understated in this transformative journey[22].
In conclusion, if you are contemplating bariatric surgery, foster a deep understanding of the surgical procedures, benefits, and associated risks backed by evidence-based information and consultation with a specialist[5]. It is a path to a healthier future, but like all significant life choices, it demands a grounded and well-informed decision, steering towards a better quality of life.
References
- World Health Organization. (2020). Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- Sjöström, L. (2013). Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. Journal of Internal Medicine, 273(3), 219–234.
- Sarwer, D. B., Wadden, T. A., & Fabricatore, A. N. (2005). Psychosocial and Behavioral Aspects of Bariatric Surgery. Obesity Research, 13(4), 639–648. https://pubmed.ncbi.nlm.nih.gov/15897471/
- Mechanick, J.I., Kushner, R.F., Sugerman, H.J. et al. (2009). American Association of Clinical Endocrinologists, The Obesity Society, and the American Society for Metabolic & Bariatric Surgery Medical Guidelines for Clinical Practice for the bariatric surgery patient’s perioperative nutritional, metabolic, and nonsurgical support. Obesity (Silver Spring), 17 Suppl 1, S1-70, V.
- Courcoulas, A. P., Christian, N. J., Belle, S. H., Berk, P. D., Flum, D. R., Garcia, L., … & Wolfe, B. M. (2013). Weight change and health outcomes three years after bariatric surgery among individuals with severe obesity. JAMA, 310(22), 2416-2425.
- American Society for Metabolic and Bariatric Surgery. (2020). Bariatric Surgery Procedures. https://pubmed.ncbi.nlm.nih.gov/35970741/
- Salminen, P., Helmio, M., Ovaska, J., Juuti, A., Leivonen, M., Peromaa-Haavisto, P., … & Victorzon, M. (2018). Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss at 5 Years Among Patients With Morbid Obesity: The SLEEVEPASS Randomized Clinical Trial. JAMA, 319(3), 241-254.
- O’Brien, P. E., Hindle, A., Brennan, L., Skinner, S., Burton, P., Smith, A., … & Brown, W. (2019). Long-Term Outcomes After Bariatric Surgery: A Systematic Review and Meta-analysis of Weight Loss at Ten or More Years for All Bariatric Procedures and a Single-Centre Review of 20-Year Outcomes After Adjustable Gastric Banding. Obesity surgery, 29(1), 3-14.
- Prachand, V. N., & Alverdy, J. C. (2010). Duodenal Switch Provides Superior Weight Loss in the Super-Obese (BMI ≥50 kg/m2) Compared With Gastric Bypass. Annals of Surgery, 252(3), 611–617.
- Buchwald H, Avidor Y, Braunwald E, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA. 2004;292(14):1724–1737. doi:10.1001/jama.292.14.1724
- Adams, T. D., Davidson, L. E., Litwin, S. E., Kim, J., Kolotkin, R. L., Nanjee, M. N., … & Hopkins, P. N. (2017). Weight and metabolic outcomes 12 years after gastric bypass. New England Journal of Medicine, 377(12), 1143-1155.
- Schauer, P. R., Bhatt, D. L., Kirwan, J. P., Wolski, K., Aminian, A., Brethauer, S. A., … & Nissen, S. E. (2017). Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. New England Journal of Medicine, 376(7), 641-651.
- Sundbom, M., Hedberg, J., Marsk, R., & Boman, L. (2017). A substantial decrease in comorbidity five years after gastric bypass: a population-based study from the Scandinavian Obesity Surgery Registry. Annals of surgery, 265(6), 1166-1171.
- Sarkhosh, K., Switzer, N. J., El-Hadi, M., Birch, D. W., Shi, X., & Karmali, S. (2013). The impact of bariatric surgery on obstructive sleep apnea: a systematic review. Obesity surgery, 23(3), 414-423.
- Kolotkin, R. L., Davidson, L. E., Crosby, R. D., Hunt, S. C., & Adams, T. D. (2018). Six-year health-related quality of life changes in gastric bypass patients versus obese comparison groups. Surgery for Obesity and Related Diseases, 8(5), 625-633. https://pubmed.ncbi.nlm.nih.gov/22386053/
- Smith, M. D., Patterson, E., Wahed, A. S., Belle, S. H., Berk, P. D., Courcoulas, A. P., … & Flum, D. R. (2011). Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obesity surgery, 21(11), 1687-1692.
- Raftopoulos, I., Martindale, C., Cronin, A., & Steinberg, J. (2004). The effect of extended post-discharge chemical thromboprophylaxis on venous thromboembolism rates after bariatric surgery: a prospective comparison trial. Surgery for Obesity and Related Diseases, 4(5), 464-471.
- Parrott, J., Frank, L., Rabena, R., Craggs-Dino, L., Isom, K. A., & Greiman, L. (2017). American Society for Metabolic and Bariatric Surgery Integrated Health Nutritional Guidelines for the Surgical Weight Loss Patient 2016 Update: Micronutrients. Surgery for obesity and related diseases, 13(5), 727-741.
- Conceição, E., de Lourdes, M., Pinto-Bastos, A., Vaz, A. R., Ramalho, S., & Brandão, I. (2017). Problematic eating behaviours and psychopathology in patients undergoing bariatric surgery: The mediating role of loss of control eating. International Journal of Eating Disorders, 50(6), 664-671.
- American Society for Metabolic and Bariatric Surgery (ASMBS). (2021). Who is a Candidate for Bariatric Surgery? Retrieved from https://asmbs.org/patients/who-is-a-candidate-for-bariatric-surgery
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (2020). Bariatric Surgery. Retrieved from https://www.niddk.nih.gov/health-information/weight-management/bariatric-surgery
- Livhits, M., Mercado, C., Yermilov, I., Parikh, J. A., Dutson, E., Mehran, A., … & Gibbons, M. M. (2011). Preoperative predictors of weight loss following bariatric surgery: systematic review. Obesity surgery, 21(1), 70-89.