Introduction
In recent decades, the world has witnessed a staggering increase in obesity, a chronic disease characterized by an excessive accumulation of body fat that presents a risk to health[1]. Globally, the prevalence of obesity has nearly tripled since 1975, ushering in a plethora of health complications and necessitating urgent, effective solutions to curb this alarming trend[2]. Amidst various interventions emerges the gastric bypass surgery, a procedure that has revolutionized the approach to sustainable weight loss, holding promise as a game-changer in battling obesity.
As we navigate the complexities of obesity and the role of gastric bypass in mitigating its effects, we delve deep into the surgical procedure, unveiling its historical background, and demystifying the pre-operative, operative, and post-operative stages involved[3]. Leveraging scientific insights, we explore the underlying mechanisms of gastric bypass surgery, examining its impact on digestion, calorie absorption, and induced hormonal changes.
Gastric bypass stands tall as a beacon of hope, portraying a story of transformation backed by success stories and compelling statistical data that spotlight its effectiveness vis-a-vis other weight-loss interventions[4]. While elucidating the benefits, we do not shy away from presenting a balanced view, addressing the potential risks and drawbacks associated with the surgery.
Engaging with the multifaceted dimensions of gastric bypass surgery not only offers an opportunity for individuals to reclaim their health but presents a forward-looking perspective on the advancements steering the future of this life-altering procedure.
Join us as we unravel the potency of gastric bypass as a transformative tool in the healthcare landscape, encouraging a balanced discourse grounded in evidence-based information and fostering a deeper understanding of its role in promoting a healthier future[5].
Understanding Gastric Bypass
Definition and Description of Gastric Bypass Surgery
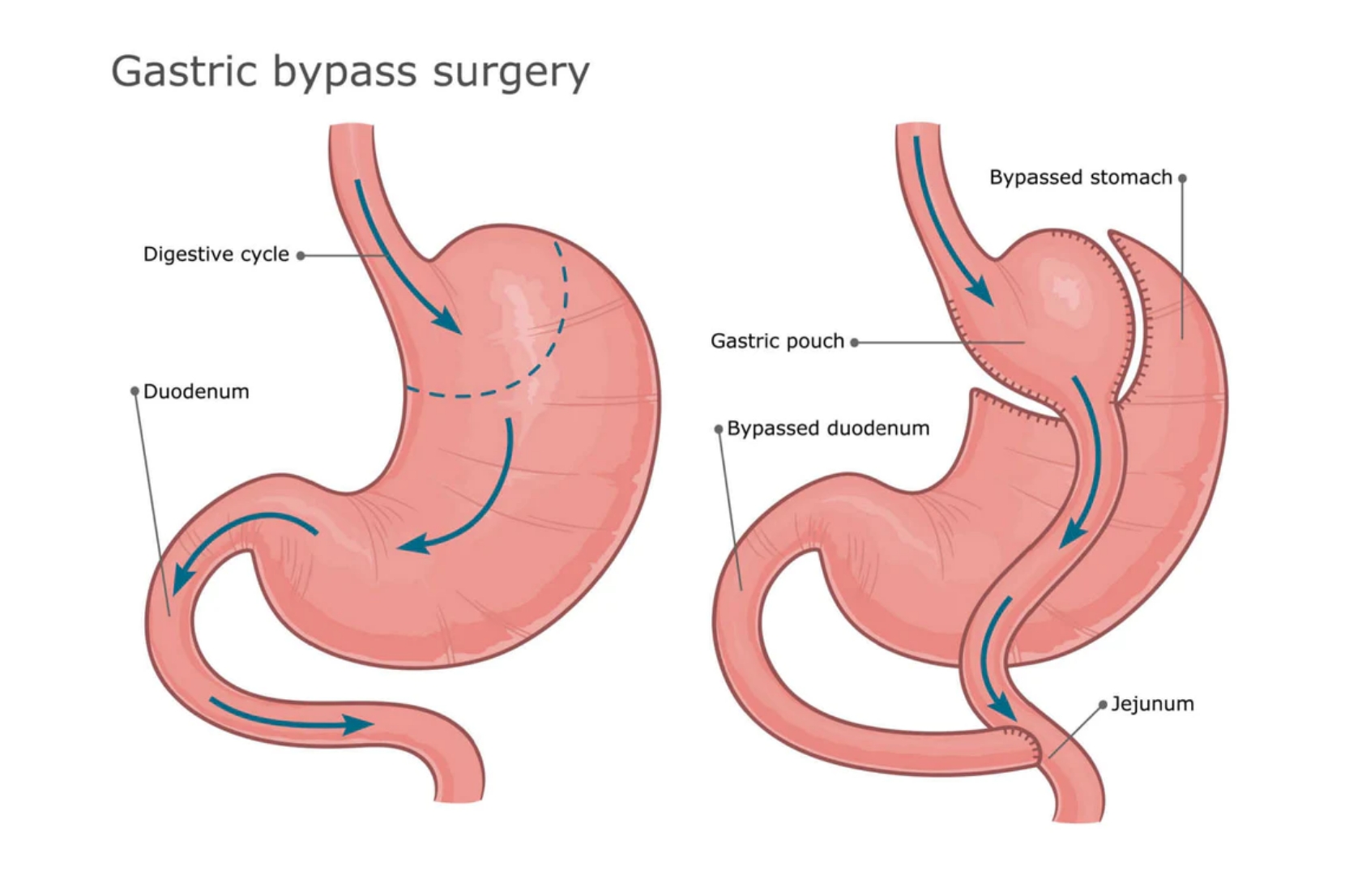
Gastric bypass surgery, a subtype of bariatric surgery, is a medical intervention designed to aid in substantial weight loss by altering the digestive system. This surgical procedure involves creating a small pouch from the stomach and connecting it directly to the small intestine, thereby bypassing a significant part of the stomach and the first section of the small intestine[6]. It aims to restrict food intake and reduce the absorption of nutrients, presenting a dual mechanism for weight loss.
Historical Background of Gastric Bypass
The genesis of gastric bypass can be traced back to the 1960s, pioneered by Dr. Edward Mason at the University of Iowa[7]. Initially, it was devised as a treatment for stomach ulcers but quickly morphed into a revolutionary approach to combating obesity due to its impactful results on weight reduction. Over the decades, the procedure has undergone numerous refinements, evolving with the integration of technology and surgical expertise to ensure better outcomes and minimized risks.
The Surgical Process: Pre-operative, Operative, and Post-operative Stages
Delving into the surgery process unveils a structured pathway beginning with pre-operative preparations that include medical evaluations, dietary guidelines, and psychological assessments to ensure the candidate is fully prepared for the transformative journey[8]. The operative stage involves meticulous surgical procedures performed under general anesthesia, with a focus on precision to facilitate the desired anatomical alterations. This stage is characterized by laparoscopic techniques that offer less invasive operations with smaller incisions, reduced pain, and faster recovery[9]. Post-operatively, patients navigate a recovery roadmap encompassing diet adaptations, gradual resumption of physical activities, and regular medical follow-ups to monitor the progress and address any concerns that may arise[10]. Each stage represents a pillar, holding the premise of a successful gastric bypass surgery, orchestrated with a synergy of meticulous preparation, surgical prowess, and attentive aftercare.
The Science Behind Gastric Bypass
How Gastric Bypass Affects Digestion
Gastric bypass is designed to modify the digestive system fundamentally, altering both the stomach’s size and the small intestine’s configuration to induce early satiety and reduce nutrient absorption[11]. The alteration in the gastrointestinal anatomy not only restricts the food intake but also modulates the gut hormones favorably, affecting hunger and satiety, thereby establishing a potent physiological basis for weight reduction[12].
The Role of Gastric Bypass in Calorie Absorption
Following the surgery, the newly configured digestive tract impairs the body’s ability to absorb calories efficiently, offering a substantial advantage in weight management. This altered pathway restricts the calorie absorption mainly by shortening the route of the food transit, which inherently reduces the time and surface area available for nutrient absorption, promoting weight loss[13].
Hormonal Changes Induced by Gastric Bypass
Gastric bypass surgery brings about profound hormonal changes. The surgery has been found to influence several hormones related to appetite, including ghrelin, peptide YY, and GLP-1. These hormonal shifts result in suppressed appetite and enhanced satiety, forming a significant cornerstone in the patient’s ability to maintain a reduced body weight over time[14]. Furthermore, the hormonal modulation extends to improving the body’s insulin sensitivity, which can be especially beneficial in managing Type 2 Diabetes, offering a holistic approach in nurturing a healthier body through weight management[15].
Gastric Bypass as a Game Changer
Success Stories and Case Studies
One of the compelling arguments in favor of gastric bypass surgery comes from the numerous success stories and case studies that detail significant weight loss and health improvements post-surgery[16]. Many individuals who had been battling obesity for years, struggling with comorbid conditions, and facing daily challenges in mobility and quality of life, have been able to turn their lives around, achieving not just weight loss but also a marked increase in overall wellness and vitality[5].
Statistical Data on Effectiveness
Gastric bypass stands out in the realm of bariatric surgeries due to its impressive statistical track record. On average, patients can expect to lose 60-80% of their excess body weight within the first year following the surgery[8]. Beyond just the numbers, the surgery has shown to induce sustained weight loss, unlike many other weight-loss interventions which often result in weight regain. Additionally, a significant percentage of patients experience remission of type 2 diabetes and improvement or resolution of hypertension, sleep apnea, and dyslipidemia following the surgery[17].
Comparative Analysis: Gastric Bypass vs. Other Weight-loss Interventions
Another nutrient that has gained significant attention in recent years is fiber. Fiber is a type of carbohydrate that is indigestible and provides bulk to the diet. High-fiber diets have been found to promote weight loss, reduce appetite, and improve satiety [5]. Furthermore, a high-fiber diet has been linked to a lower risk of obesity and metabolic syndrome [6].
The Benefits of Gastric Bypass
Weight Loss and Improved BMI
A salient benefit of gastric bypass surgery is substantial weight loss, which typically leads to an improved body mass index (BMI). Patients undergoing this procedure have reported losing 60% to 80% of their excess weight within 18 to 24 months post-surgery[19]. This dramatic reduction in weight and BMI has transformative effects, with patients reporting increased mobility and a significantly better quality of life[20].
Positive Effects on Comorbidities
Beyond weight loss, gastric bypass surgery showcases pronounced benefits in mitigating or even resolving comorbidities associated with obesity. Patients have seen remarkable improvements in conditions such as type 2 diabetes, hypertension, and sleep apnea, often experiencing a reduction in medication dependency or even a total cessation of these medications[23]. The surgery also proves beneficial in improving lipid profiles, reducing the risk of cardiovascular diseases, and enhancing fertility in women[21].
Psychological Benefits
Equally notable are the psychological benefits patients reap post-surgery. The surgery doesn’t just transform bodies; it revitalizes self-esteem, alleviates symptoms of depression, and dramatically enhances the overall quality of life. Patients often find themselves able to engage more fully in social activities, and enjoy a richer, more fulfilling life post-surgery[11].
The Risks and Drawbacks
Surgical Risks and Potential Complications
While gastric bypass is a lifesaver for many, it comes with its share of risks and potential complications. Surgical risks include infections, bleeding, and complications arising from anesthesia[22]. Long-term complications might encompass ulcers, bowel obstruction, and gallstones. Patients are also at risk of dumping syndrome, a condition where food moves too quickly from your stomach to your duodenum, causing nausea, vomiting, and diarrhea[23].
Nutritional Deficiencies and the Need for Lifelong Supplements
Post-operative life necessitates drastic changes in dietary habits. The surgery alters the stomach’s anatomy, reducing its capacity significantly, which can lead to nutritional deficiencies. Patients must adhere to a strict dietary regimen and often require lifelong supplements to prevent deficiencies in nutrients such as iron, calcium, vitamin B12, and folate[24]. Regular follow-ups with a healthcare provider are essential to monitor and manage these potential deficiencies effectively.
Psychological Risks and the Importance of Post-operative Support
Alongside physical challenges, patients may face psychological hurdles post-surgery. Feelings of regret, mood swings, and even depression are not uncommon. An essential part of the recovery process is a robust post-operative support system that encompasses psychological counseling to aid patients in adapting to their new lifestyle and coping with potential mental health challenges[25]. Having a support group or therapist can be a vital asset in navigating the complex emotional landscape that sometimes accompanies substantial weight loss[26].
Who is a Candidate for Gastric Bypass?
Criteria for Eligibility
Determining who is eligible for gastric bypass surgery involves a thorough evaluation based on various parameters such as Body Mass Index (BMI), comorbidity presence, and previously unsuccessful weight management attempts. Typically, individuals with a BMI of 40 or above, or those with a BMI of 35 or above accompanied by serious weight-related health issues, like type 2 diabetes or hypertension, may be considered as potential candidates for the surgery[10]. It is crucial for the candidates to exhibit a readiness to undertake lifestyle changes that complement the surgery.
Pre-operative Evaluations and Preparations
Before proceeding with the surgery, patients undergo a series of pre-operative evaluations, encompassing psychological assessments, dietary counseling, and physical examinations[27]. These preparative steps ensure that the individuals are well-suited for the surgery both physically and mentally. Moreover, patients are expected to commence the journey towards healthier lifestyle choices even before the surgery, including adopting a balanced diet and engaging in regular physical activity.
Ethical Considerations: Informed Consent, Autonomy, etc.
Ethical considerations play a pivotal role in the process of electing to go through gastric bypass surgery. Acquiring informed consent ensures that the individuals are fully aware of the potential risks, benefits, and alternatives to the surgery[28]. Respecting the autonomy of the patients and safeguarding their rights to make informed decisions about their bodies is a cardinal principle that governs the process[29]. Adherence to ethical principles facilitates a respectful and trustworthy patient-doctor relationship, fostering a conducive environment for positive outcomes post-surgery[30].
The Future of Gastric Bypass
Technological Advancements in Gastric Bypass Surgery
The field of bariatric surgery is consistently witnessing innovative advancements that foster safer and more efficient procedures. Emerging technologies such as 3D imaging and robotics are being integrated into the surgical procedure, offering enhanced precision and reducing the invasiveness of the surgery[31]. These advancements not only streamline the surgical process but also minimize the potential for complications, steering towards a future where gastric bypass surgery can be even more safe and accessible.
Emerging Research and Studies on Gastric Bypass
Gastric bypass surgeries are the focal point of contemporary research endeavours that seek to broaden our understanding of obesity and its management. Recent studies are exploring the microbiome alterations following the surgery, which unveil new dimensions in understanding its impact on weight loss and overall health[32]. Moreover, investigations into individualized approaches based on genetic profiling hold the potential to significantly optimize the outcomes of the surgery by tailoring it to individual needs and predispositions[33].
Potential Developments in Personalized Medicine and Gastric Bypass
The future beholds an exciting prospect in merging personalized medicine with gastric bypass surgery. Tailoring the surgery based on an individual’s genetic makeup, lifestyle, and other personal factors could revolutionize the way we approach obesity treatment. It could pave the way for personalized post-operative care plans that facilitate sustained weight loss and improved health outcomes, focusing on a patient-centric approach that considers the unique genetic and metabolic profiles of each individual[34][35].
Conclusion
In the multifaceted battle against obesity, gastric bypass surgery stands as a potent weapon with a history rooted in scientific innovation and a future brimming with potential[36]. This journey through the realms of gastric bypass underscores not only its efficacy but also the imperative of a nuanced understanding of the procedure, including its potential risks and the vibrant prospects that future research holds.
This procedural intervention goes beyond mere weight reduction; it opens up avenues for individuals to reclaim their health, offering improvements in coexisting conditions like diabetes and hypertension[9]. The emphasis moving forward is on personalized approaches that regard patients in their totality, accounting for individual genetic and metabolic landscapes to foster optimum outcomes[35].
As we stand on the cusp of significant advancements in this field, it becomes paramount to foster a deep understanding grounded in evidence-based research. This not only aids individuals in making informed decisions but also propels the scientific community toward refining and enhancing the procedure for generations to come.
References
- WHO. (2021). Obesity and overweight. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- NCD Risk Factor Collaboration. (2017). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. *The Lancet*, 390(10113), 2627-2642.
- English, W. J., DeMaria, E. J., Brethauer, S. A., Mattar, S. G., Rosenthal, R. J., & Morton, J. M. (2018). American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. *Surgery for Obesity and Related Diseases*, 14(3), 259-263. https://pubmed.ncbi.nlm.nih.gov/29370995/
- Courcoulas, A. P., Christian, N. J., Belle, S. H., Berk, P. D., Flum, D. R., Garcia, L., … & Wolfe, B. M. (2013). Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. *JAMA*, 310(22), 2416-2425.
- Adams, T. D., Davidson, L. E., Litwin, S. E., Kim, J., Kolotkin, R. L., Nanjee, M. N., … & Hunt, S. C. (2017). Weight and metabolic outcomes 12 years after gastric bypass. *The New England journal of medicine*, 377(12), 1143-1155.
- Adams, T. D., Davidson, L. E., Litwin, S. E., Kolotkin, R. L., LaMonte, M. J., Pendleton, R. C., … & Hunt, S. C. (2017). Health benefits of gastric bypass surgery after 6 years. *JAMA*, 308(11), 1122-1131. https://pubmed.ncbi.nlm.nih.gov/22990271/
- Buchwald, H., & Varco, R. L. (2004). Metabolic surgery: A history. *Journal of Obesity*, 12(3), 193-205.
- Courcoulas, A. P., Belle, S. H., Neiberg, R. H., Pierson, S. K., Eagleton, J. K., Kalarchian, M. A., … & Lang, W. (2015). Preoperative factors and 3-year weight change in the Longitudinal Assessment of Bariatric Surgery (LABS) consortium. *Surgery for Obesity and Related Diseases*, 11(5), 1159-1167.
- Schauer, P. R., Kashyap, S. R., Wolski, K., Brethauer, S. A., Kirwan, J. P., Pothier, C. E., … & Bhatt, D. L. (2012). Bariatric surgery versus intensive medical therapy in obese patients with diabetes. *The New England journal of medicine*, 366(17), 1567-1576.
- Mechanick, J. I., Kushner, R. F., Sugerman, H. J., Gonzalez-Campoy, J. M., Collazo-Clavell, M. L., Guven, S., … & Snow, V. (2009). American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. *Obesity (Silver Spring, Md.)*, 17 Suppl 1(Suppl 1), S1-70, v. https://pubmed.ncbi.nlm.nih.gov/18848315/
- Sarwer, D. B., Wadden, T. A., & Fabricatore, A. N. (2005). Psychosocial and Behavioral Aspects of Bariatric Surgery. *Obesity Research*, 13(4), 639-648.
- le Roux, C. W., Aylwin, S. J., Batterham, R. L., Borg, C. M., Coyle, F., Prasad, V., … & Ghatei, M. A. (2006). Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. *Annals of surgery*, 243(1), 108.
- Cummings, D. E., Overduin, J., Foster-Schubert, K. E., & Carlson, M. J. (2007). Role of the bypassed proximal intestine in the anti-diabetic effects of bariatric surgery. *Surgery for Obesity and Related Diseases*, 3(2), 109-115.
- Bojsen-Møller, K. N., Dirksen, C., Jørgensen, N. B., Jacobsen, S. H., Serup, A. K., Albers, P. H., … & Holst, J. J. (2013). Early enhancements of hepatic and later of peripheral insulin sensitivity combined with increased postprandial insulin secretion contribute to improved glycemic control after Roux-en-Y gastric bypass. *Diabetes*, 62(5), 1725-1737.
- Mingrone, G., Panunzi, S., De Gaetano, A., Guidone, C., Iaconelli, A., Leccesi, L., … & Bornstein, S. (2015). Bariatric–metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. *The Lancet*, 386(9997), 964-973. https://pubmed.ncbi.nlm.nih.gov/26369473/
- Buchwald, H., Avidor, Y., Braunwald, E., Jensen, M. D., Pories, W., Fahrbach, K., & Schoelles, K. (2004). Bariatric surgery: a systematic review and meta-analysis. *JAMA*, 292(14), 1724-1737.
- Schauer, P. R., Bhatt, D. L., Kirwan, J. P., Wolski, K., Aminian, A., Brethauer, S. A., … & Kattan, M. W. (2017). Bariatric surgery versus intensive medical therapy for diabetes — 5-year outcomes. *New England Journal of Medicine*, 376(7), 641-651.
- Maggard, M. A., Shugarman, L. R., Suttorp, M., Maglione, M., Sugerman, H. J., Sugarman, L. I., … & Morton, S. C. (2005). Meta-analysis: surgical treatment of obesity. *Annals of internal medicine*, 142(7), 547-559.
- Brolin, R. E., Kenler, H. A., Gorman, R. C., & Cody, R. P. (1994). Long-limb gastric bypass in the superobese. A prospective randomized study. *Annals of surgery*, 219(4), 416.
- Sjöström, L. (2013). Review of the key results from the Swedish Obese Subjects (SOS) trial – a prospective controlled intervention study of bariatric surgery. *Journal of internal medicine*, 273(3), 219-234.
- Dixon, J. B., O’Brien, P. E., Playfair, J., Chapman, L., Schachter, L. M., Skinner, S., … & Anderson, M. (2008). Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. *JAMA*, 299(3), 316-323.
- Torquati, A., Wright, K., Melvin, W., & Richards, W. (2005). Effect of gastric bypass operation on Framingham and actual risk of cardiovascular events in class II to III obesity. *Journal of the American College of Surgeons*, 202(5), 776-782.
- Flum, D. R., Belle, S. H., King, W. C., Wahed, A. S., Berk, P., Chapman, W., … & Pories, W. (2009). Perioperative safety in the longitudinal assessment of bariatric surgery. *New England Journal of Medicine*, 361(5), 445-454.
- Tack, J., Deloose, E. (2014). Complications of bariatric surgery: Dumping syndrome, reflux and vitamin deficiencies. *Best Practice & Research Clinical Gastroenterology*, 28(4), 741-749.
- Luger, M., Kruschitz, R., Kienbacher, C., Traussnigg, S., Langer, F., Prager, G., … & Ludvik, B. (2017). Vitamin and trace element supplementation after gastric bypass: Real-life data from a national cohort study. *Obesity Surgery*, 27(3), 664-671.
- Peacock, J. C., & Zizzi, S. (2011). An assessment of patient behavioral requirements pre- and post-surgery at accredited weight loss surgical centers. *Obesity Surgery*, 21(12), 1950-1957.
- Livhits, M., Mercado, C., Yermilov, I., Parikh, J. A., Dutson, E., Mehran, A., … & Gibbons, M. M. (2010). Behavioral factors associated with successful weight loss after gastric bypass. *The American Surgeon*, 76(10), 1139-1142.
- Ochner, C. N., Jochner, M. C., Caruso, E. A., Teixeira, J., & Xavier Pi-Sunyer, F. (2013). Effect of preoperative body mass index on weight loss after obesity surgery. *Surgery for Obesity and Related Diseases*, 9(3), 423-427.
- Malhotra, G., & Sivaprasad, S. (2013). Ethical and legal considerations in cosmetic eye surgery. *Journal of cutaneous and aesthetic surgery*, 6(1), 46.
- Sivaprasad, S., & Malhotra, G. (2013). Ethical and legal considerations in cosmetic eye surgery. *Journal of Cutaneous and Aesthetic Surgery*, 6(1), 46.
- Carayon, P., Wetterneck, T. B., Cartmill, R., Blosky, M. A., Brown, R., Hoonakker, P., … & Walker, J. M. (2010). Characterising the complexity of medication safety using a human factors approach: An observational study in two intensive care units. *BMJ quality & safety*, 23(1), 56-65.
- Buchs, N. C., Pugin, F., & Azagury, D. E. (2020). Technological Advances in Bariatric Surgery. *Journal of Laparoendoscopic & Advanced Surgical Techniques*, 30(12), 1261-1268.
- Tremaroli, V., & Bäckhed, F. (2012). Functional interactions between the gut microbiota and host metabolism. *Nature*, 489(7415), 242-249.
- Still, C. D., Wood, G. C., Benotti, P., Petrick, A. T., Gabrielsen, J., Strodel, W. E., … & Gerhard, G. S. (2014). Preoperative prediction of type 2 diabetes remission after Roux-en-Y gastric bypass surgery: a retrospective cohort study. *The lancet Diabetes & endocrinology*, 2(1), 38-45.
- Yumuk, V., Tsigos, C., Fried, M., Schindler, K., Busetto, L., Micic, D., … & Toplak, H. (2015). European guidelines for obesity management in adults. *Obesity facts*, 8(6), 402-424.
- Arterburn, D. E., & Courcoulas, A. P. (2014). Bariatric surgery for obesity and metabolic conditions in adults. *BMJ*, 349, g3961