Introduction
Obesity is an escalating global health concern that poses severe risks to an individual’s well-being[1]. Over the years, with changing lifestyle dynamics and dietary habits, there’s been a marked increase in individuals seeking medical and surgical interventions to combat obesity. Weight loss surgeries or bariatric procedures are among the most trusted and sought-after solutions. These surgeries offer an effective means of weight reduction for those who have struggled with other conventional methods, such as dieting and exercise[2].
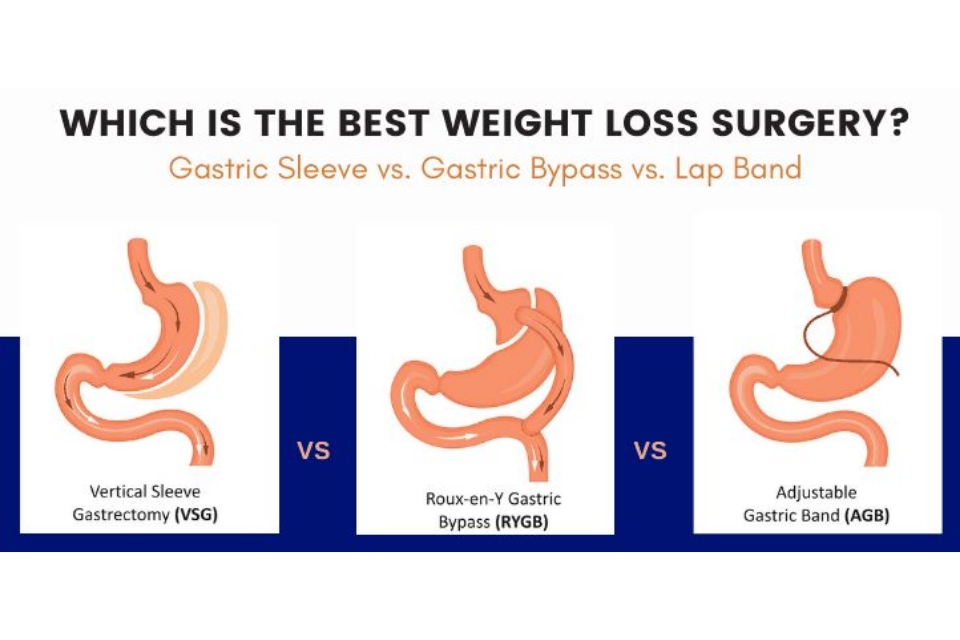
While several types of weight loss surgeries are available, making an informed choice can be daunting. Gastric Bypass, one of the most well-known bariatric surgeries, is frequently weighed against other procedures like the Gastric Sleeve, Adjustable Gastric Banding, and Biliopancreatic Diversion with Duodenal Switch[3]. Each has its merits, complications, and suitability criteria. The primary objective of this article is to provide readers with a comprehensive comparison between Gastric Bypass and its counterparts, aiding in making a well-informed decision tailored to individual needs[4].
As we delve deeper into the intricacies of these surgeries, it’s imperative to approach the subject with an open mind and understand that the ‘best’ option may vary significantly from one individual to another, depending on numerous factors, including health status, weight loss objectives, and dietary commitments post-surgery[5].
Gastric Bypass Surgery (Roux-en-Y Gastric Bypass)
Gastric Bypass surgery, precisely the Roux-en-Y procedure, remains one of the most widely recognised and executed bariatric surgeries worldwide[6].
Advantages
The efficacy of the Roux-en-Y Gastric Bypass can be attributed to several key advantages. One of the most notable benefits is the rapid and significant weight loss patients often experience, typically more pronounced than many other surgical alternatives[7]. Additionally, there’s the potential for an improvement or even cure of obesity-related conditions, such as type 2 diabetes and hypertension, which positions this surgery as a weight-loss tool and a health improvement strategy[8]. Moreover, a distinct advantage is the alteration in gut hormones, resulting in reduced appetite and enhanced feelings of fullness or satiety[9].
Disadvantages
However, like all medical interventions, Gastric Bypass surgery has its challenges. Being a complex procedure, there is an inherent potential for more significant complications than less invasive bariatric surgeries[10]. One of the primary concerns post-surgery is the possibility of nutrient and vitamin deficiencies, making it essential for patients to adhere to dietary guidelines and, in many cases, lifelong supplementation. Another notable drawback is its non-reversibility, which means the changes made during the procedure are permanent.
Gastric Sleeve (Sleeve Gastrectomy)
The Gastric Sleeve, or Sleeve Gastrectomy, has recently gained immense popularity as an effective alternative to more complex bariatric procedures[11].
Advantages
The core mechanism of the Gastric Sleeve procedure involves removing a significant portion of the stomach, specifically the part responsible for producing the hunger-stimulating hormone ghrelin. This naturally results in reduced food intake and helps to curtail excessive feelings of hunger[12]. One of the standout benefits of this surgery is its relative simplicity, especially when compared to the Gastric Bypass, which involves rerouting the intestines. As there’s no intestinal bypass, concerns about vitamin and mineral deficiencies are comparatively lower, making post-surgical dietary management somewhat less stringent[13].
Disadvantages
While the Gastric Sleeve presents several advantages, it’s not devoid of drawbacks. Firstly, the procedure is irreversible; once a portion of the stomach is removed, it cannot be restored. This permanency requires potential candidates to consider the long-term implications carefully. Another aspect worth noting is that, in some cases, the weight loss resulting from a Sleeve Gastrectomy may be less substantial than what one might achieve with a Gastric Bypass, particularly in the long run[14]. Additionally, as with any surgery, there are potential risks and complications, such as leakage at the surgical site or the development of gastric reflux[15].
Adjustable Gastric Banding (Lap Band)
Adjustable Gastric Banding, commonly known as the Lap Band procedure, offers a less invasive alternative to other weight loss surgeries and employs a distinct mechanism for managing obesity[16].
Advantages
The Lap Band procedure involves placing an adjustable silicone band around the upper portion of the stomach. The band creates a smaller stomach pouch, thus restricting the amount of food consumed and promoting a sensation of fullness with lesser food intake[17]. A significant advantage of this procedure is its reversibility. If complications arise or the patient decides to remove it, the band can be adjusted or even wholly removed without permanent anatomical changes[18]. Moreover, since there’s no alteration or rerouting of the intestines, the risk of vitamin and nutrient deficiencies is substantially reduced compared to other bariatric procedures[19].
Disadvantages
However, Lap Band surgery isn’t without limitations. Many patients experience slower and, at times, less weight loss than other surgical methods. Potential complications specific to the band include slipping, erosion into the stomach, or mechanical issues with the band itself, which could necessitate further interventions or removal[20]. Another concern is the necessity for regular follow-up appointments to adjust the band’s tightness based on weight loss progress and comfort, which requires a long-term commitment from the patient.
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
Among the repertoire of weight loss surgeries, the Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is one of the most complex yet often highly effective procedures for morbid obesity[21].
Advantages
The BPD/DS is primarily known for achieving the most significant weight loss among all bariatric surgeries. It combines restrictive (reducing the size of the stomach) and malabsorptive (reducing calorie absorption in the intestines) elements, making it exceptionally potent in its efficacy[22]. The result is substantial weight reduction and notable improvements in comorbid conditions such as type 2 diabetes, sleep apnea, and hypertension, often surpassing the outcomes of other surgeries[23]. Furthermore, due to the preservation of the stomach’s pyloric valve and the beginning of the duodenum, patients tend to experience fewer complications related to ulcers or dumping syndrome.
Disadvantages
The complexity of BPD/DS also brings about a range of disadvantages. Firstly, the potential for severe malnutrition and vitamin deficiencies is heightened due to the decreased absorption of nutrients[24]. Lifelong adherence to dietary supplements and regular monitoring are critical post-surgery. Another concern is the increased risk of foul-smelling stools and flatus, a side effect of unabsorbed fats. Additionally, given the intricacy of the procedure, potential candidates must choose surgeons with significant experience in BPD/DS, as the risk of surgical complications can be higher compared to other bariatric procedures[25].
Factors to Consider When Choosing a Procedure
Deciding on the right bariatric surgery is not a one-size-fits-all scenario. Several pivotal considerations should guide this decision, ensuring that the chosen method aligns with the individual’s health profile, weight loss goals, and tolerance for potential risks[26].
Health Status and Comorbid Conditions
One’s overall health and the presence of obesity-related conditions, like type 2 diabetes or sleep apnea, can significantly influence the choice of surgery. Some procedures offer enhanced outcomes for specific conditions. For instance, BPD/DS and Gastric Bypass might provide better resolution for type 2 diabetes than Gastric Banding[27].
Desired Weight Loss and Maintenance
The expected amount and duration of weight loss vary between procedures. While BPD/DS might lead to the most significant reduction, Gastric Banding often results in slower and sometimes lesser weight loss. Individuals’ motivation and commitment to post-surgical lifestyle changes also affect long-term weight maintenance[8].
Potential Risks and Post-operative Lifestyle
Every procedure carries its set of potential complications and requires distinct post-operative care. For example, while Gastric Bypass might offer rapid weight loss, it also poses risks of nutrient deficiencies, necessitating lifelong supplements. Conversely, the Gastric Band requires periodic adjustments and monitoring but is less invasive[29]. Evaluating one’s willingness to adapt to the post-operative dietary, exercise, and medical follow-up requirements is crucial.
Consultation with Experts
Lastly, a thorough discussion with bariatric surgeons and attending informational seminars can provide insights into the most suitable procedure. Often, a patient’s unique circumstances and the surgeon’s expertise will jointly dictate the most appropriate surgical path[30].
Conclusion
Selecting the ideal weight loss surgery is a momentous decision, requiring careful consideration of various factors, including health status, weight loss objectives, potential risks, and the willingness to embrace post-operative changes[31].
Each procedure presents its unique set of advantages and drawbacks, whether it’s the Gastric Bypass, Gastric Sleeve, Lap Band, or BPD/DS. Studies suggest that while surgical methods offer notable weight loss and health improvements, success and sustainability largely depend on the individual’s commitment to a transformed lifestyle post-surgery[3]. Moreover, with the medical landscape constantly evolving, staying informed about the latest research and advancements is paramount[33].
A comprehensive consultation with a seasoned bariatric surgeon remains invaluable, ensuring that the chosen surgical route aligns with the individual’s health aspirations and life circumstances[7]. Regardless of the selected procedure, embracing the journey with informed choices and unwavering dedication can pave the way for a healthier and more fulfilling life[35].
References
- World Health Organization (WHO). “Obesity: Preventing and Managing the Global Epidemic.” Geneva: World Health Organization, 2000.
- Sjöström, L. “Bariatric surgery and long-term cardiovascular events.” *JAMA*, 2012; 307(1):56-65.
- Buchwald, H., & Oien, D. M. “Metabolic/bariatric surgery worldwide.” *Obesity Surgery*, 2013; 23(4):427-436.
- Maggard-Gibbons, M. et al. “Bariatric surgery for weight loss and glycemic control in non-morbidly obese adults with diabetes: a systematic review.” *JAMA*, 2013; 309(21):2250-2261.
- Courcoulas, A. P. et al. “Weight change and health outcomes at three years after bariatric surgery among patients with severe obesity.” *JAMA*, 2013; 310(22):2416-2425.
- DeMaria, E.J. et al. “Validation of the obesity surgery mortality risk score in a multicenter study proves it stratifies mortality risk in patients undergoing gastric bypass for morbid obesity.” *Annals of Surgery*, 2007; 246(4):578-584.
- Schauer, P.R., et al. “Bariatric surgery versus intensive medical therapy for diabetes — 3-year outcomes.” *The New England Journal of Medicine*, 2014; 370:2002-2013.
- Adams, T.D., et al. “Long-term mortality after gastric bypass surgery.” *The New England Journal of Medicine*, 2007; 357(8):753-761.
- le Roux, C.W., et al. “Gastric bypass reduces fat intake and preference.” *American Journal of Physiology-Regulatory, Integrative and Comparative Physiology*, 2011; 301(4):R1057-R1066.
- Flum, D.R., et al. “Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures.” *JAMA*, 2005; 294(15):1903-1908.
- Rosenthal, R.J., et al. “International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on the experience of >12,000 cases.” *Surgery for Obesity and Related Diseases*, 2012; 8(1): 8-19.
- Cummings, D.E., et al. “Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery.” *The New England Journal of Medicine*, 2002; 346(21):1623-1630.
- Bohdjalian, A., et al. “Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin.” *Obesity Surgery*, 2010; 20(5): 535-540.
- Benaiges, D. et al. “Laparoscopic sleeve gastrectomy and laparoscopic gastric bypass are equally effective for reducing cardiovascular risk in severely obese patients at one year of follow-up.” *Surgery for Obesity and Related Diseases*, 2011; 7(5): 575-580.
- Aurora, A.R., et al. “Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients.” *Surgical Endoscopy*, 2012; 26(6): 1509-1515.
- O’Brien, P.E., et al. “Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomised trial.” *Annals of Internal Medicine*, 2006; 144(9): 625-633.
- Dixon, J.B., et al. “Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomised controlled trial.” *JAMA*, 2008; 299(3): 316-323.
- Fielding, G.A., & Allen, J.W. “A step-by-step guide to placement of the LAP-BAND adjustable gastric banding system.” *American Journal of Surgery*, 2002; 184(6B): 26S-30S.
- Favretti, F., et al. “Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results.” *Obesity Surgery*, 2007; 17(2): 168-175.
- Himpens, J., et al. “Long-term outcomes of laparoscopic adjustable gastric banding.” *Archives of Surgery*, 2011; 146(7): 802-807.
- Marceau, P., et al. “Biliopancreatic diversion with duodenal switch.” *World Journal of Surgery*, 1998; 22(9): 947-954.
- Prachand, V.N., & Alverdy, J.C. “Duodenal switch provides superior resolution of metabolic comorbidities independent of weight loss in the super-obese (BMI ≥ 50 kg/m2) compared with gastric bypass.” *Journal of Gastrointestinal Surgery*, 2010; 14(2): 211-220.
- Topart, P., Becouarn, G., & Ritz, P. “Weight loss is more sustained after biliopancreatic diversion with duodenal switch than Roux-en-Y gastric bypass in superobese patients.” *Surgery for Obesity and Related Diseases*, 2013; 9(4): 526-530.
- Skroubis, G., et al. “Roux-en-Y gastric bypass versus a variant of biliopancreatic diversion in a non-superobese population: prospective comparison of the efficacy and the incidence of metabolic deficiencies.” *Obesity Surgery*, 2006; 16(4): 488-495.
- Søvik, T.T., et al. “Weight loss, cardiovascular risk factors, and quality of life after gastric bypass and duodenal switch: a randomised trial.” *Annals of Internal Medicine*, 2011; 155(5): 281-291.
- Courcoulas, A.P., et al. “Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial.” *JAMA Surgery*, 2014; 149(7): 707-715.
- Mingrone, G., et al. “Bariatric surgery versus conventional medical therapy for type 2 diabetes.” *The New England Journal of Medicine*, 2012; 366(17): 1577-1585.
- Dixon, J.B., & O’Brien, P.E. “Health outcomes of severely obese type 2 diabetic subjects 1 year after laparoscopic adjustable gastric banding.” *Diabetes Care*, 2002; 25(2): 358-363.
- Maggard, M.A., et al. “Meta-analysis: surgical treatment of obesity.” *Annals of Internal Medicine*, 2005; 142(7): 547-559.
- Sjöström, L., et al. “Effects of bariatric surgery on mortality in Swedish obese subjects.” *The New England Journal of Medicine*, 2007; 357(8): 741-752.
- Arterburn, D.E., et al. “Intensive lifestyle intervention vs. gastric bypass for type 2 diabetes: an interim analysis of a randomized controlled trial.” *Obesity*, 2013; 21(11): 2372-2379.
- Colquitt, J.L., et al. “Surgery for weight loss in adults.” *Cochrane Database of Systematic Reviews*, 2014; (8): CD003641.